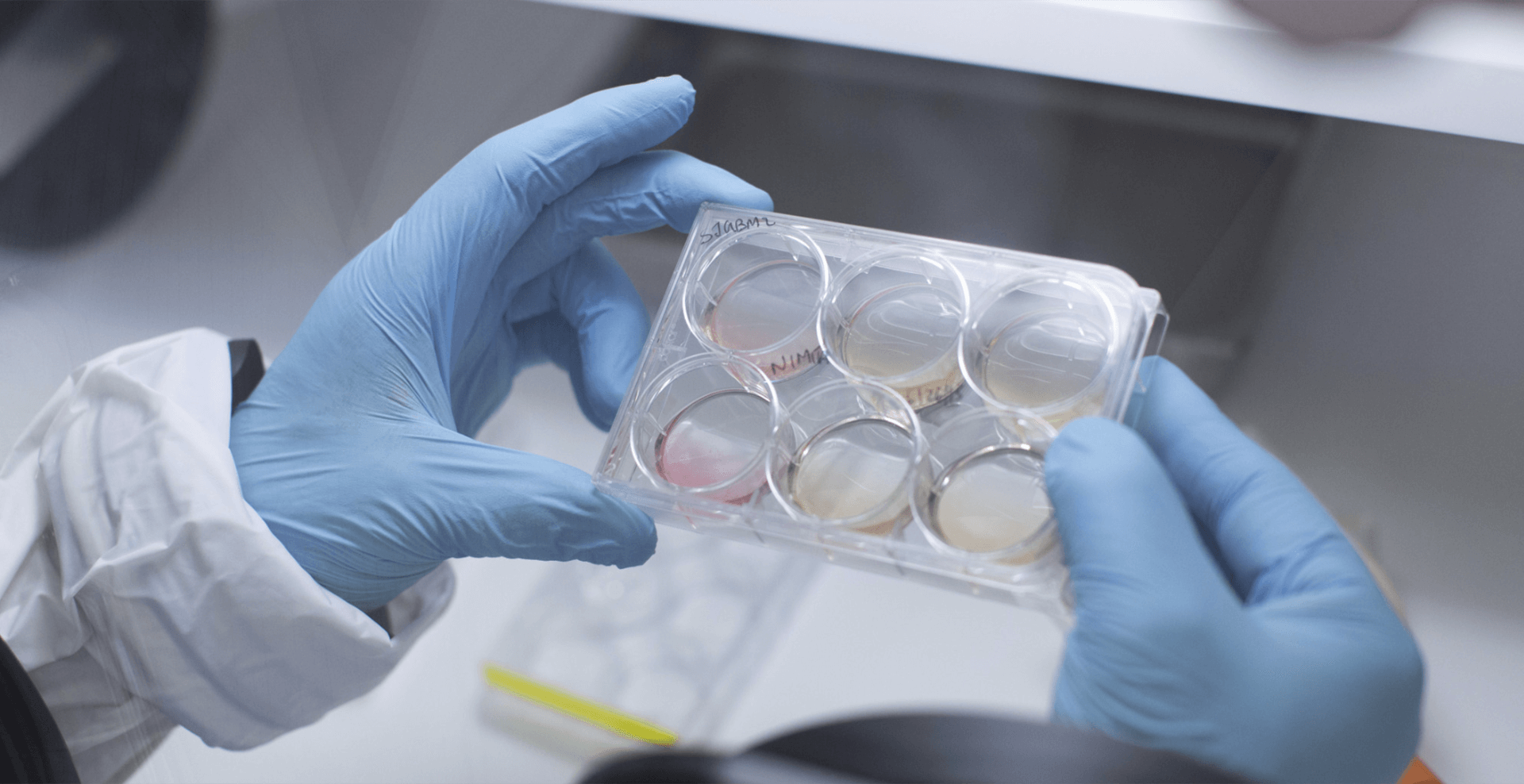
In the Department of Microbiology and Immunology at IU School of Medicine, research centers on molecular mechanisms of pathogenesis, immune responsiveness, infectious diseases, cancer biology, hematopoiesis, stem cell biology and gene therapy. Current research activities include microbial pathogenesis and experimental therapeutics, with a focus on host-pathogen interactions in the extracellular niche, mechanisms of oncogenic pathogens, the role of the microbiome in human disease, and the molecular and cellular biology of obligate intracellular viral and bacterial pathogens. Investigators place a major emphasis on immunology, including studies of immune responsiveness, immune evasion by viruses and tumors, innate and adaptive immunity, antigen presentation, and B cell responses.

Education
Department faculty teach foundational and advanced courses for medical and graduate students and mentor medical students, graduate students and postdoctoral fellows in topical and advanced biomedical research.
Learn More Education

Research
The department’s research on stem cells, hematopoiesis, transplantation and hematological malignancies is among the best—and most funded by NIH—in the United States.
Learn More Research

Faculty
Departmental faculty conduct well-funded research in molecular pathogenesis, immunology, hematopoiesis and gene transfer while educating the next generation of scientists and physicians in these fields.
Learn More Faculty
17
Primary Faculty
8
Million in Annual Research Funding
4
Focus Areas of Research
Training the Next Generation of Medical Scientists
Faculty in the Department of Microbiology and Immunology train PhD students in cutting-edge biomedical research; the department also offers a research-based MS degree designed to prepare students for advanced technical careers or to be competitive for subsequent PhD study.
Research Expertise
Twenty-one primary and 21 secondary faculty in this department together offer research expertise in a broad diversity of topics ranging from basic to clinical and translational research in immunology, pathogenesis, hematopoiesis, stem cell biology, gene therapy and cancer biology.